Coding will be instrumental to your agency’s success under PDGM. Performing an audit of your coding practices now will provide the opportunity to educate your staff on accurate and cohesive coding guidelines and targeted aspects of the OASIS to ensure you are prioritizing both patient needs and accurate reimbursement.
PDGM Coding Guidelines
Principle Diagnosis, as reflected on the claim, will determine the clinical grouping factor under PDGM. Clinical groupings include:
1. Musculoskeletal Rehabilitation
2. Neuro/Stroke Rehabilitation
3. Wounds
4. Complex Nursing Interventions
5. Behavioral Health Care
6. Medication Management, Teaching and Assessment (MMTA) – Surgical Aftercare
7. MMTA – Cardiac/Circulatory
8. MMTA – Endocrine
9. MMTA – Gastrointestinal/Genitourinary (GI/GU)
10. MMTA – Infectious Disease/Neoplasms/Blood-forming Diseases
11. MMTA – Respiratory
12. MMTA – Other
Secondary Diagnosis on the claim will drive comorbidity adjustments:
A. No Adjustments: No secondary dx/comorbidities that fall into subgroups
B. Low Adjustment: A 30-day period of care would receive a low comobidity adjustment if there is one reported secondary diagnosis that falls within one of these 13 home-health specific individual comorbidity subgroups:
1. Neuro 11: diabetic retinopathy and other blindness
2. Neuro 10: peripheral and polyneuropathies
3. Circulatory 9: acute and chronic embolisms and thrombosis
4. Heart 11: heart failure
5. Cerebral 4: sequelae of cerebral vascular diseases
6. Neuro 5: Parkinson’s disease
7. Skin 1: cutaneous abscess, cellulitis, lymphangitis
8. Neuro 7: hemiplegia, paraplegia, and quadriplegia
9. Circulatory 10: varicose veins with ulceration
10. Skin 3: diseases of arteries, arterioles, capillaries w/ulceration & non-pressure, chronic ulcers
11. Skin 4: stages two through four and unstageable pressure ulcers
12. Heart 10: cardiac dysrhythmias
13. Neoplasms 01: Oral cancers
C. High Adjustment: A 30-day period of care would receive a high comorbidity adjustment if there are two or more reported secondary diagnoses that fall within one or more of the comobidity subgroup interactions.
OASIS Coding
OASIS coding will drive functional levels in conjunction with clinical groupings. There are three functional levels: Low, Medium, and High. These are directly correlated to functional impairment with Low being the highest functioning patients, and High being the lowest functioning patients.
Points will be assigned based on responses to the following OASIS questions:
1. M1800: Grooming
2. M1810: Current ability to dress upper body
3. M1820: Current ability to dress lower body
4. M1830: Bathing
5. M1840: Toilet transferring
6. M1850: Transferring
7. M1860: Ambulation/Locomotion
8. M1022: Risk for hospitalization (at least 3 responses checked, excluding #8, #9, #10)
Thresholds for each functional level have been established by clinical grouping: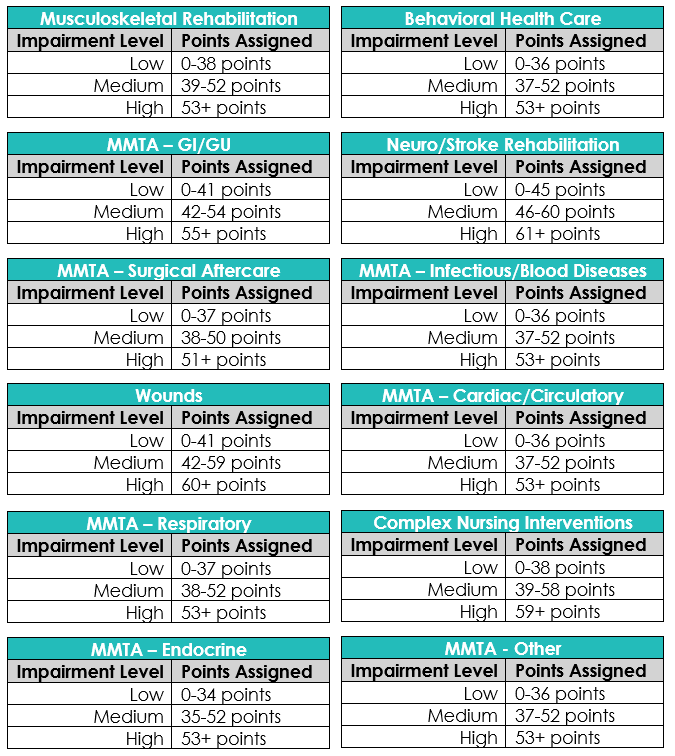
Reviewing your agency’s current ICD-10 codes in relation to the new clinical groupings and determining the potential for comorbidity adjustments is a very impactful and an important exercise to consider as you prepare for PDGM. HealthPRO Heritage at Home is prepared to help you execute and succeed in the transition to PDGM! We understand the changes that are required and have the resources and ability to support your agency’s success.


