With PDGM on the horizon in less than 100 days, agencies are hearing more chatter around three key areas: Face-to-Face (F2F) Encounters, Targeted Probe and Educate (TPE), and Review Choice Demonstration (RCD). All three will affect reimbursement as agencies will need to utilize best practices. Agencies must thoroughly understand the requirements of each process to sustain viability going forward.
Face-to-Face (F2) Encounter: According to CMS guidelines, the Face-to_face must identify the following:
- A skilled need stating that the patient will benefit from home health services for the disciplines ordered (SN, PT, OT, and ST).
- Documentation that the patient is homebound. The criteria for a patient to be homebound includes: any mental/physical condition that restricts the ability of the individual to leave his or her home except with the assistance of another individual or the aid of a supportive device (such as crutches, a cane, a wheelchair or a walker). And/ or if the individual has a condition such that leaving his or her home is medically contraindicated and leaving home requires a considerable and taxing effort by the individual.
- The Face-to-Face Encounter must be the most recent physician visit note/assessment that reflects the current need for skilled services and the most current clinical condition/ physical status of the patient. Pre-op notes and medical clearances for a procedure will not suffice.
- If the encounter has been completed but does not contain the above components, the physician must complete an “Addendum to the Face-to-Face”. The Face-to-Face encounter and any addendums must be signed and dated by the physician.
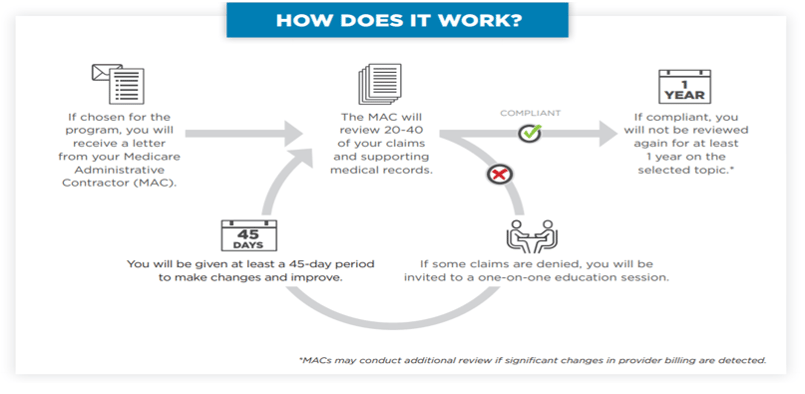
Targeted Probe and Educate (TPE): PDGM will likely put agencies under the microscope with providing timely, accurate, and appropriate care. The TPE program was designed to help providers and suppliers reduce claim denials and appeals through one-on-one help. We hope that most providers will not have to face a TPE, but having the appropriate and required documentation is essential under PDGM.
Four of the most common claims errors to avoid are listed below:
- The signature of the certifying physician was not included in the claim.
- The face-to-face encounter notes did not support all elements of eligibility.
- Documentation did not meet or prove medical necessity.
- The claim had missing or incomplete initial certifications or recertifications.
Review Choice Demonstration (RCD): This demonstration establishes the review choice process for home health services to assist in developing improved procedures to identify and prevent fraud, protect beneficiaries from harm, and safeguard taxpayer dollars to empower patients while minimizing unnecessary provider burden. The demonstration helps ensure that the right payments are made at the right time for home health service through either pre-claim or post payment review. It protects Medicare funding from improper payments, reduces the number of Medicare appeals, and improves provider compliance with Medicare program requirements. HHAs will select from three initial choices:
- Pre-claim review,
- Post payment review, or
- Minimal post payment review with a 25% payment reduction.
After a 6-month period, HHAs demonstrating compliance with Medicare rules through pre-claim review or post payment review will have additional choices, including relief from most reviews except for a review of a small sample of claims. CMS has provided us with a Demonstration Process Flow Sheet. They have also included a Review Decision Flowchart for reference as well.
HealthPRO Heritage is dedicated to helping you become more aware and educated on the payment reform facing agencies. Please reach out to us at homehealth@healthpro-heritage.com if you have any questions or ideas on how we can help your agency.
Click here for the printable version.
Flowchart above courtesy of CMS.

