Value-Based Purchasing (VBP) will go into effect on January 1, 2023. The model incentivizes quality of care improvements while ensuring there is no limitation in coverage for Medicare beneficiaries and includes updated payment rates and reimbursement to Home Health Agencies (HHAs).
This model has a maximum adjustment of ± 5%, with average performance compared to other HHAs in their cohort receiving no adjustment. Competing HHAs that demonstrate they can deliver a higher quality of care in a given performance year measured against a baseline year relative to peers nationwide, could have their HH PPS claims final payment amount adjusted higher than the amount that otherwise would be paid. Competing HHAs that do not perform as well as other competing HHAs in the same volume-based cohort might have their HH PPS claims final payment amount reduced. In addition, competing HHAs that perform similarly to others in the same volume-based cohort might have no payment adjustment. By expanding the HHVBP model in 2023, CMS seeks to improve the beneficiary experience by providing incentives for Medicare Certified Home Health Agencies to provide a better quality of care with greater efficiency.
Does This Include All Agencies?
The proposed model will include all agencies and will divide HHAs into two cohorts:
- Larger-volume HHAs that receive 40 or more completed HHCAHPS surveys in a performance year
- Smaller-volume HHAs that receive fewer than 40 completed surveys.
Agencies will be compared to others in their cohort beginning CY 2023 and subsequent years.
When does VBP go into effect?
There are three time periods for VBP.
- Baseline Year: The year against which measured performance in a performance year will be compared.
- Performance Year: The calendar year during which data are collected for the purpose of calculating a competing HHA’s performance on measures.
- Payment Year: The calendar year in which the applicable percent, a maximum upward or downward adjustment, applies.
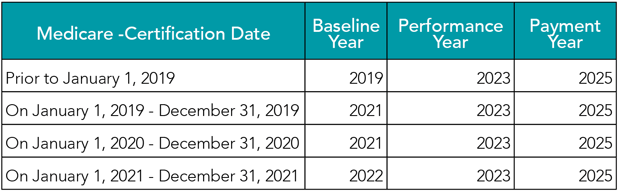
Each of these time periods is based on your individual agency’s Medicare certification date as identified in the table below.
How does VBP work?
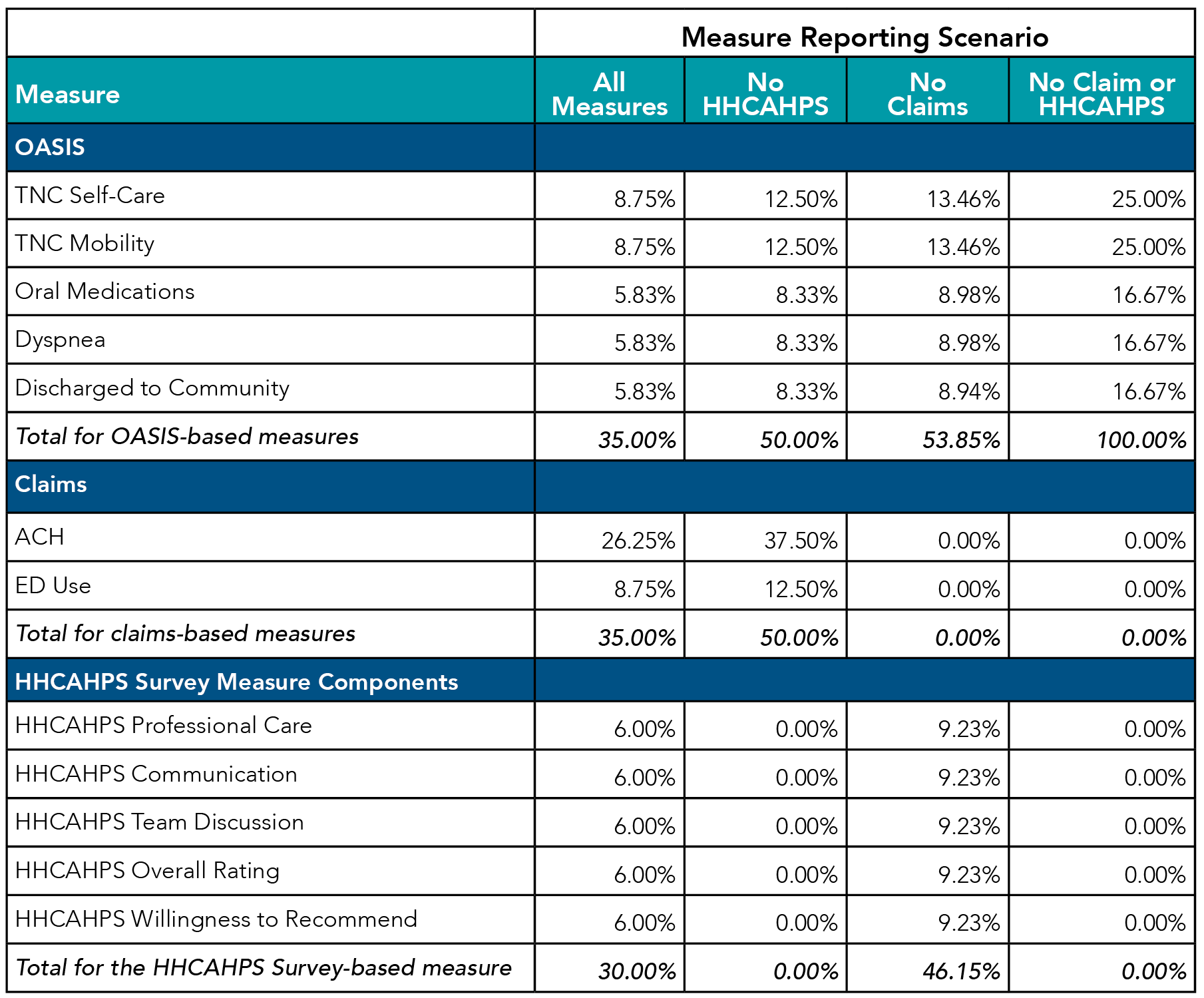
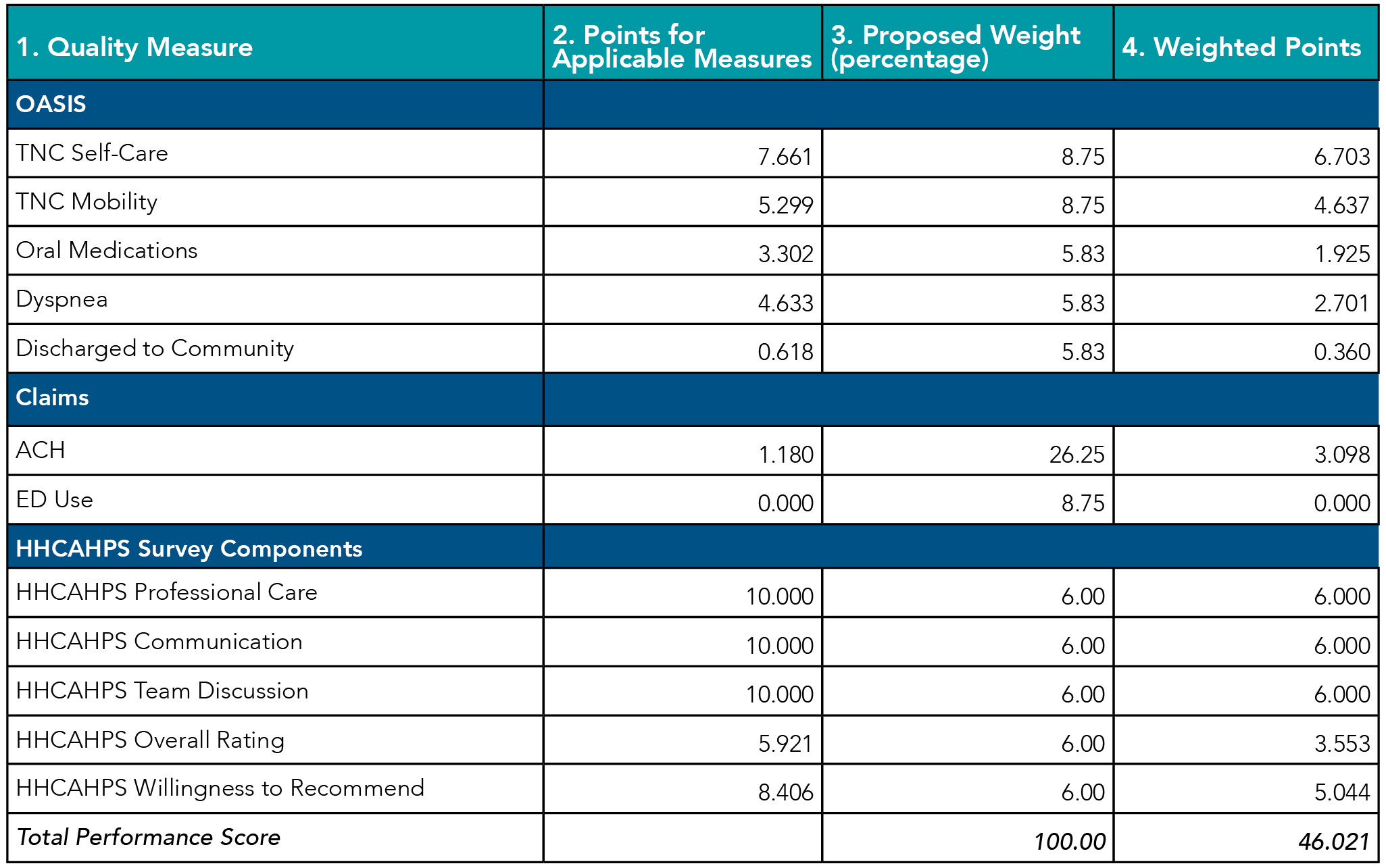
Value-Based Purchasing is driven by your agency's performance. More specifically, CMS will use data already reported by HHAs, to form a Total Performance Score (TPS). There are three categories that make up the TPS: OASIS (35% of TPS), Claims (35% of TPS), and HHCAHPS survey data (30% of TPS). The individual metrics that comprise each of the three categories within the TPS are listed in the table below. It is worth noting that Hospitalization during the First 60 Days of Home Health Use (ACH), as part of the Claims measure, makes up more than one-quarter of the entire TPS score. While self-care and mobility scoring make up the largest percentage of the OASIS data, at 8.75% each.
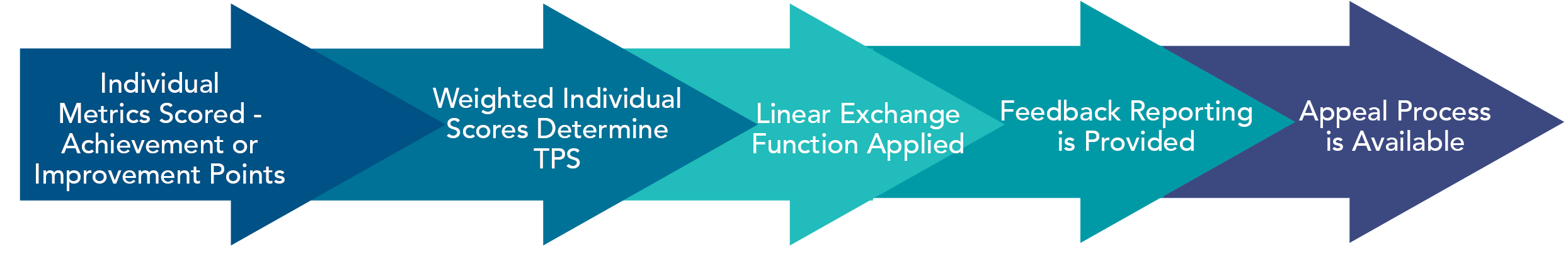
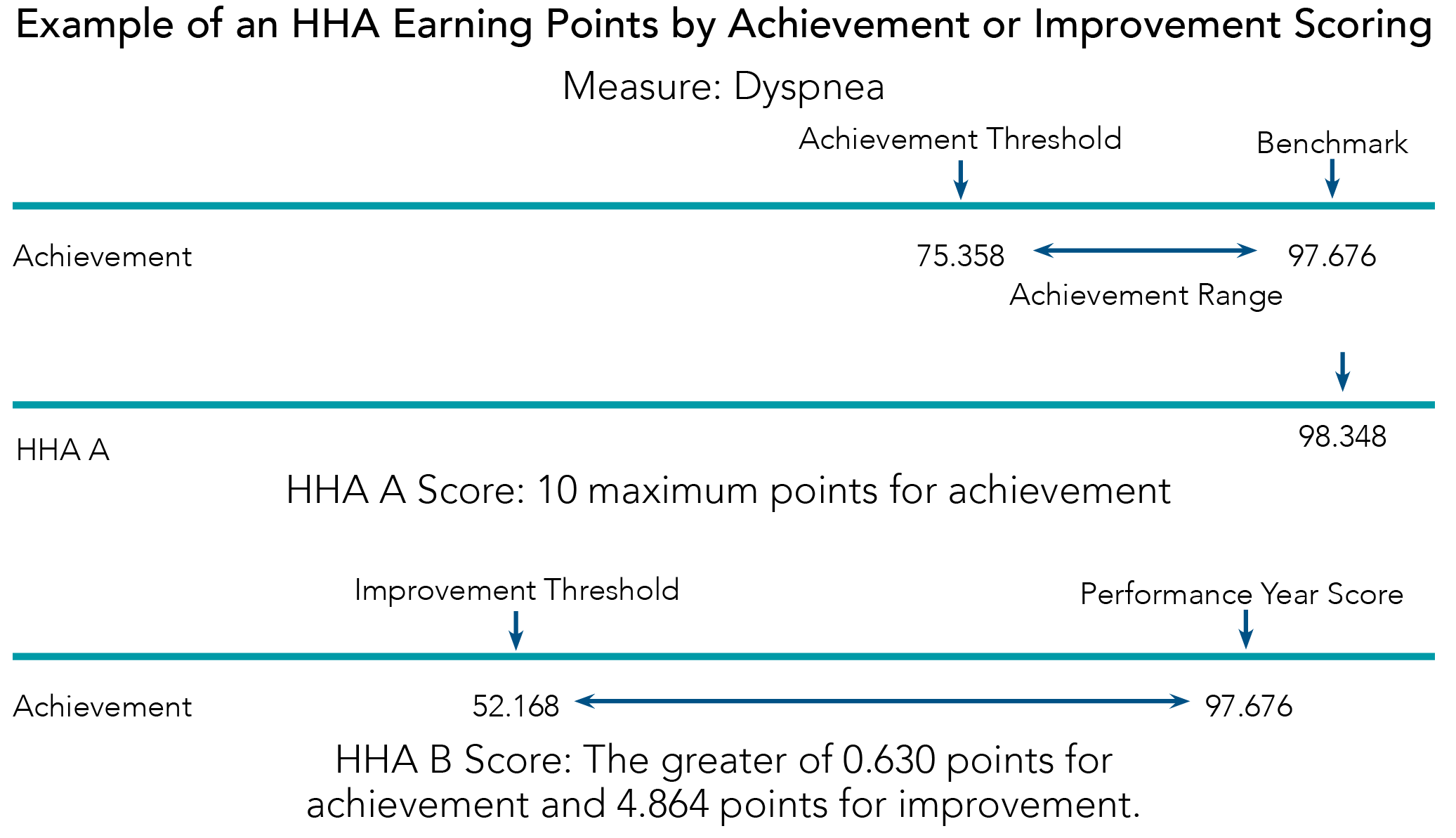
Each individual measure within the three categories is scored independently using the higher of Achievement Points or Improvement Points. Up to 10 Points can be awarded for Achievement and Up to 9 for Improvement for each measure.
After each individual measure is scored they are weighted based on their individual percentage of the overall score and the weighted sum of the performance scores forms the Total Performance Score, ranging from 0 to 100.
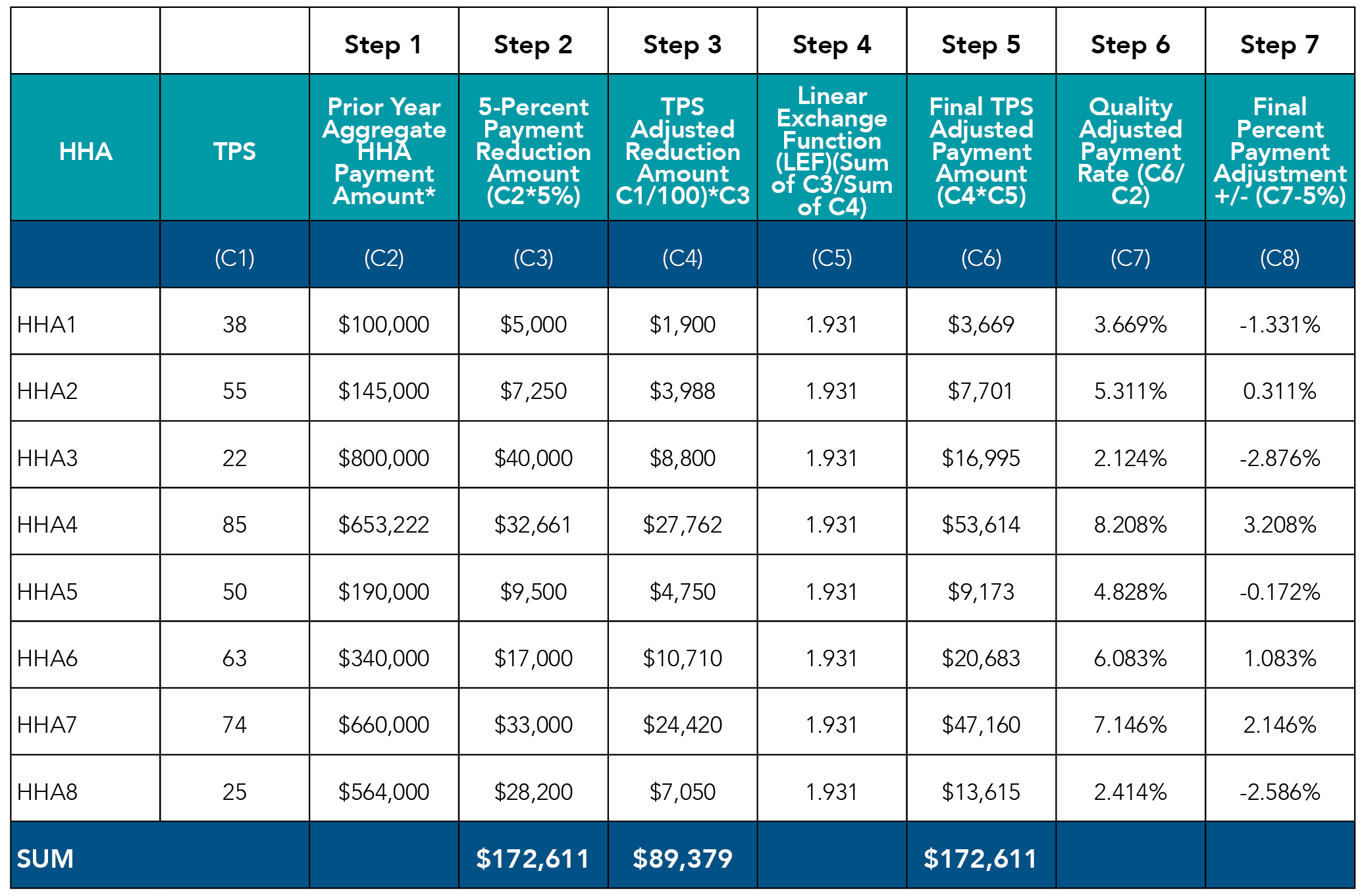
The Total Performance Score (TPS) for each HHA is then used for a Linear Exchange Function (LEF) calculation to determine the adjustments for the “payment” years. As seen in the table below, using this equation each agency’s value-based incentive payment amount for a fiscal year will depend on the Total Performance Score and the amount of an agency's base operating HHRG payment amount.
The value-based incentive payment adjustment (Step 7/C8 in the table below) will be applied as an adjustment to the base operating HHRG payment amount for each agency’s episodic payment in the “payment year”.
Performance Feedback Reports
Reporting will be available to agencies on a regular basis to provide feedback on performance and projected reimbursement impacts.
- Interim Performance Report (IPR) - Provides feedback to HHAs regarding performance in both achievement and improvement within their applicable nationwide cohort
- Distributed Quarterly - the first one will be issued in July 2023
- Includes 12 most recent months of data
- Provides feedback regarding both achievement and improvement performance
- Both preliminary and final Interim Performance Reports will be issued
- Annual TPS and Payment Adjustment Report-3 versions
- Preview Annual Report – confidential review of scores and adjustments. If you disagree with the data, you can request a recalculation within 15 days and a Preliminary Annual Report will be issued. If no request for recalculation is made, then a Preliminary Annual Report will not be issued.
- Preliminary Annual Report (if applicable) if agencies appeal their data
- Final Annual Report – issued before the start of the payment adjustment year
Below is a timetable outlining the timelines for the Performance Feedback Reports.
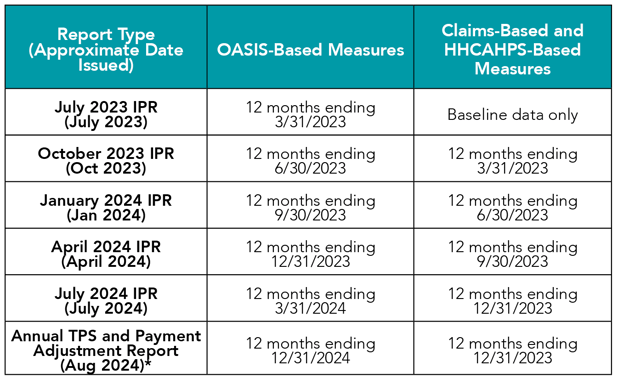
*The Annual Report made available to HHAs in approximately August 2024 is the Preview Annual Report. The Final Annual Report is issued after the recalculation and reconsideration request periods and no later than 30 days prior to the calendar year which the payment adjustment will take effect.
As you can determine from the information above, Value-Based Purchasing is a complex model to understand and operationalize within your Home Health agency.
For additional support and expert insight regarding Value-Based Purchasing, contact HealthPRO Heritage at Home at homehealth@healthpro-heritage.com. We are here to answer questions you may have and provide support to ensure your success in 2022 and beyond.

