Gut-Check Survey Results + Feedback from the PDPM Front Line
HealthPRO Heritage launched a survey – “PDPM Gut-Check” – to capture how the industry is feeling about the new reimbursement system. Here’s what you and your peers had to say.
When asked what worries them about PDPM, the majority of respondents say they are concerned about coding accuracy as well as potential audits and documentation pitfalls. Many also cited that potential cut-backs in therapy are a major concern as well, while providers with in-house therapy are worried about “finding the right balance of minutes to achieve the patient outcomes needed.”
 Have you heard about the industry’s only virtual ICD-10 outsourced coding service for SNFs? Available from HealthPRO Heritage in partnership with himagine Solutions, this unique coding service offers (much-needed) coding support for dozens of SNFs nationwide who have already enrolled. The feedback so far is overwhelmingly positive; we are feeling the love!
Have you heard about the industry’s only virtual ICD-10 outsourced coding service for SNFs? Available from HealthPRO Heritage in partnership with himagine Solutions, this unique coding service offers (much-needed) coding support for dozens of SNFs nationwide who have already enrolled. The feedback so far is overwhelmingly positive; we are feeling the love!
“I never imagined coding to be as complicated as it is. Our team simply coded just based on our best assumptions. Thanks to this coding service, we don’t worry, and we are in a much better place!”
“We appreciate this coding expertise! Our facility benefits from having an expert coding all our charts, and we also get answers to our questions to help us understand the why.”
“This coding service has been a huge help to our facility! We now have coding support for all our new admissions as well as our long term charts after the provider visits.”
When asked how they will measure success under PDPM, several respondents expressed uncertainty: “Unclear!” “No idea!” While many others stated they will judge success based on their team’s ability to produce outcomes and/or optimize reimbursement. (Stay tuned for more on this topic from HealthPRO Heritage in an upcoming blog/white paper RE: “Measuring Success in the New Era of PDPM.”)
When asked about the potential upside of PDPM, one respondent enthusiastically replied, “Demonstrating to the world that skilled nursing facilities have always been capable of caring holistically for residents!” Others responding to the survey see opportunity for better reimbursement (as with caring for more complex residents.)
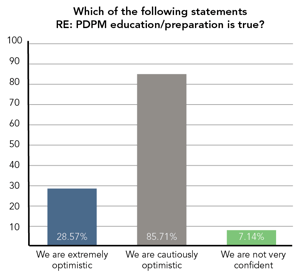
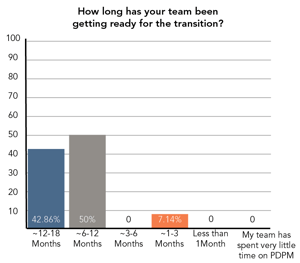
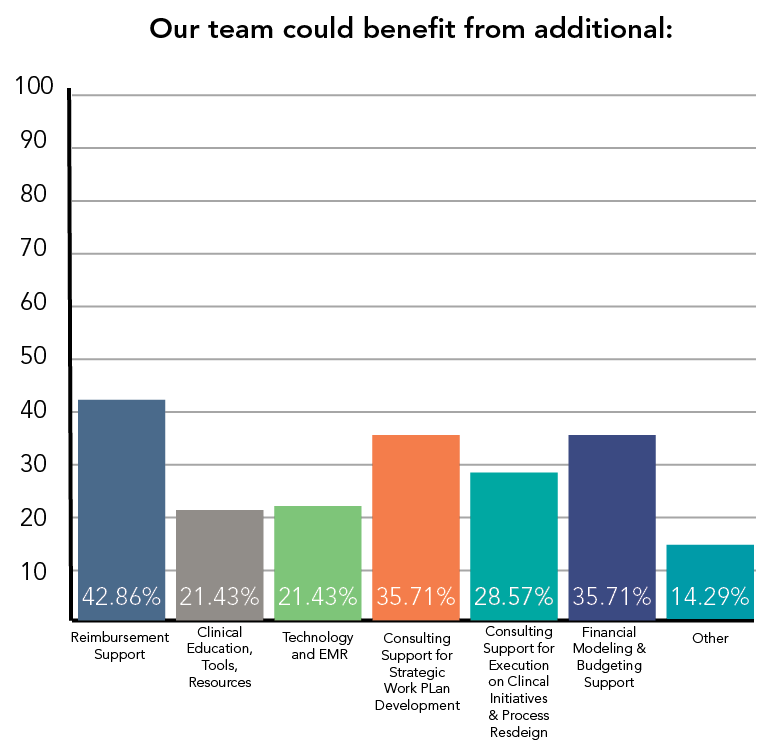
Scroll down* for more interesting survey responses illustrated below. Spoiler alert! While most have been doing their homework to prepare for PDPM, there are still important issues to tackle!
Finger on the Pulse: With 2 weeks under our belts, HealthPRO Heritage continues to provide boots-on-the-ground support for clients from coast to coast.
 Our Clinical Strategies Team has fielded ~400 calls via the ever-so-valuable 24/7 hotline service: TeleMDS. Interesting to note: The most common questions from the field are very specific and related to correct coding procedures and assigning NTA points appropriately. Keep the calls coming; we love hearing from the front lines.
Our Clinical Strategies Team has fielded ~400 calls via the ever-so-valuable 24/7 hotline service: TeleMDS. Interesting to note: The most common questions from the field are very specific and related to correct coding procedures and assigning NTA points appropriately. Keep the calls coming; we love hearing from the front lines.
Tips & Tricks From the Foxhole: HealthPRO Heritage’s Kristy Yoskey (SVP, Clinical Strategies/PDPM Task Force) sat in on several “PDPM huddles” to support the interdisciplinary teams in the trenches during the first two weeks of PDPM. All the teams earned high praise for their #PDPMReadiness, but we did note some common pitfalls. Please warn your front line staff of the following:
ALWAYS be sure to…
- Use the CMS ICD-10 Mapping Tool during the PDPM huddle to assure capture of all possible NTA items that are necessary to be capture in section I8000 of the MDS. We are seeing these being overlooked when coding.
- Understand how Section GG impacts capture for the Nursing category. Specifically, know that higher functioning scores on GG could negatively impact the Nursing category. For example – as with Parkinson’s Disease – if the functional score >11, the resident will not fit in the special care low category.
- Look to see whether signs and/or symptoms of a swallowing disorder are documented in the medical record within 7 days of the ARD. Note: it’s not necessary for a specific diagnosis to be documented to capture credit. and only requires one day in that 7 day lookback to capture.
NEEDED: Strategies & Solutions for…
- Working closely with physicians on diagnosis coding. Specifically, how do we handle a physician’s change if/when after the code has been resolved on Day 2 or Day 3? Ask yourself: Are we still monitoring the condition? Are there still labs or medications ordered for this same condition?
- Consistent documentation to assure ongoing communication to nursing staff. For example, how do we alert the nursing team RE: updates to NTAs, changes in required nursing skills and new primary diagnoses?
- Additional training RE: Optional IPAs. Universally, the IDT may not be focused on which factors might warrant a change in a PDPM first tier classification. “This is not at all surprising since the teams are focusing only on admissions right now as they wrap their heads around their new PDPM workflows,” comments Ms. Yoskey.
Over-Sharing is Okay: Please share your comments and insights here on our blog, and/or reach out to HealthPRO Heritage if your team is looking for additional education, strategy and/or tools for PDPM & Beyond! We are so proud and happy to report on how encouraged we are by the success stories from our staff and clients RE: the PDPM transition. We look forward to sharing more insights and best practices as the next few weeks and months unfold. Reach out at info@healthpro-heritage.com if you have any questions or further insights.
Additional results from our gut-check survey: