It seems everyone’s roles are changing with the onset of PDPM. Even referring clinicians (MDs, NPs and PAs) who send their patients to a skilled nursing facility will need to commit to a new more comprehensive, faster-paced process.
We’re all familiar with today’s common conundrum: The H&P sent from the referring hospital is often limited…sometimes vague…and hardly provides for a comprehensive clinical picture. Under PDPM, optimal reimbursement for SNFs hinges on whether referring clinicians do their part to help change this frustrating hurdle.
Consider that – within the first two days of a Medicare Part A stay – enough data must be provided to determine the nursing skilled services, clinical category for PT/OT and SLP, and identify 36 of the Non-Therapy Ancillary (NTA) comorbid conditions and extensive services as well as the SLP related comorbid conditions. For optimal coding, coders must capture accurate, up-to-date clinical data derived from:
- The initial physician assessment to include diagnoses (pre-admission), and
- Timely, subsequent ongoing assessments.
But most clinicians are not accustomed to providing such detailed diagnoses in their medical notes. So, how can SNFs best collaborate with their referring clinical partners to introduce this new process?
HealthPRO Heritage offers the following strategies to assist SNFs in defining necessary collaboration between referring clinicians:
- Accelerate timing of data capture: Initial MD admission assessment must be completed within 48 hours after admission
- Increase coding specificity when documenting diagnoses
- Ensure IDT workflow for ICD-10 coding is collaborative (nursing, MDS, therapy, social service and dietary)
- Adopt flexibility in coding processes to allow new codes added and/or resolved within the EMR to capture the most up-to-date picture for the 5-day and potential Interim Payment Assessments (IPAs)
- Demonstrate interdisciplinary cooperation on changes in condition to support the most active/up-to-date care plan with orders, labs, medications, and diagnoses in support of current services/interventions
- Create new processes/useful tools for MDs to increase compliance, such as:
- A template for the MD notes to capture relevant clinical details (e.g.: surgical history, etc.)
- A ‘hot list’ of the most common RTP codes (especially symptom codes) to be avoided
- Consider having MDs write out the diagnoses and then subsequently have coders translate MD notes to proper corresponding ICD-10 codes
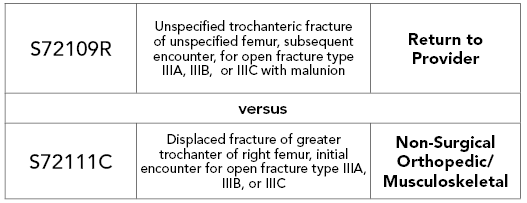
- Understand the implications of coding choices. Example to illustrate the repercussions of choosing one code versus another:
HealthPRO Heritage also offers the following internal tips for SNFs:
- Set up a pre-admission process to gather as much diagnostic intel as possible
- Redesign clinical meetings (daily clinical & weekly discharge planning) to obtain the most up-to-date and complete information
- Involve all practitioners throughout the resident’s stay
- Review documentation & new orders (e.g.: for medications & lab work) for evidence that supports the SNF stay
- Start now! Preparation for the transition to PDPM is a process that takes time. Integrating this culture change ASAP for MDs and other referral sources as best practice will prepare teams for PDPM, assure optimal reimbursement, and improve communication and ultimately patient care
- Rely on HealthPRO Heritage for support. Choose the right partner who can add value across the clinical & reimbursement landscape. As much a clinical strategy consultant as a progressive therapy partner, HealthPRO Heritage is well-positioned for the future to help SNFs successfully transition to PDPM and differentiate their performance in an ever-increasing competitive environment. If you haven’t already, NOW is the time to consider the advantage of a partner – like HealthPRO Heritage – with an earned reputation for seeing “The Big Picture” of what it takes to be successful in a highly competitive, quality-driven marketplace
#WeAreReady to guide/support your community before, during, and after payment reform transition occurs. Contact us for PDPM Consulting and/or Therapy Services: info@healthpro-heritage.com

