As PDGM edges closer, there is rising concern and tension around the submission of claims that contain primary diagnoses that do not fall into one of the 12 clinical groupings established by CMS. Such primary diagnoses are known as "Questionable Encounters" (QEs). QE codes are "too vague," meaning the code did not provide adequate information to support the need for home health services. CMS listed 43,287 eligible primary diagnoses codes in their PDGM Grouper Tool.
Under PDGM, claims for QEs will be sent back to the agency as "Return to Provider" (RTP) since CMS will not be able to assign the 30-day period to one of the 12 PDGM clinical groups.
Examples of the Top 25 QE Codes:
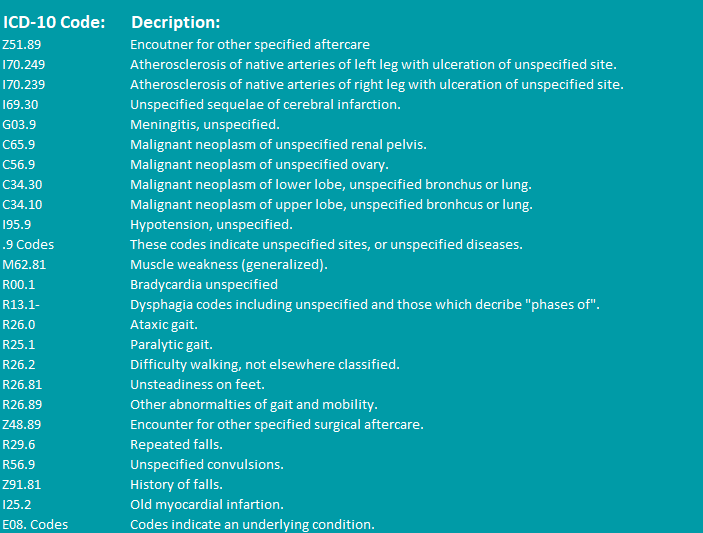 CMS is projecting that approximately 15% of episodes will not fit into a clinical grouping, based on 2017 submitted data. Around 60% of the QE codes submitted were found to be on the chart listed above. As of right now this is not the final ruling on the list of codes, these can change before final ruling
CMS is projecting that approximately 15% of episodes will not fit into a clinical grouping, based on 2017 submitted data. Around 60% of the QE codes submitted were found to be on the chart listed above. As of right now this is not the final ruling on the list of codes, these can change before final ruling
How to Decrease Questionable Encounters:
- Improve the referral intake, documentation, quality assurance and coding process within each agency. Clarify the need for precise and specific documentation and diagnosis coding with your referral sources. For example, if the patient has generalized muscle weakness due to inactivity because of COPD, then COPD is to be coded. The muscle weakness would be apparent by documentation such as manual muscle testing scores, functional assessment findings, and observations noted in the clinical narrative notes. Another example is instead of “gait abnormality” the coding should reflect lower extremity osteoarthritis or the medical reason that is causing the gait abnormality.
- Educate your referral intake team to recognize diagnosis codes that will not be associated with a clinical grouping. Also, be able to provide education to referral sources behind the reason for more specific diagnosis coding and documentation in order to decrease or eliminate a return to provider claim. Also, a RTP is not a denial of payment, but rather an opportunity to review and resubmit a claim with more appropriate and justified primary diagnosis codes.
- Clinical documentation practices are imperative to support patient complexity, homebound status, and skilled need. CMS expects clinicians to investigate the cause of symptom codes, obtain provider confirmation, and assign that code.
- Review your current coding trends and any diagnosis that will fall under a questions encounter with PDGM. Take action now to begin to eliminate use of these codes. Educate your staff on appropriate coding in preparation for these upcoming changes with focus on ensuring treatment plans are centered . This will involve educating your clinical team to make sure that their treatment plan is centered on the source of the disease or impairment, rather than the symptoms alone.
- Avoid using unspecified codes, coding etiology before manifestation, symptom codes as the primary code, inappropriate acute conditions, and diagnosis codes not supporting the need for homecare.
Due to PDGM’s classification system, care coordination and management will become vitally important. Home health providers will need to establish improved interdisciplinary collaboration processes involving both nursing and therapy teams. Remember, the primary diagnosis submitted on the claim will be the only factor that determines an episode’s clinical grouping. Therefore, it is important to research questionable encounters now and make sure your agency is coding correctly. Now is the time to begin to investigate the potential impact PDGM will have on your overall reimbursement due to your coding practices. We are here to help at HealthPRO Heritage.


